Page 13 <previous page > <next page>
SOME HEALTH & SCIENCE NEWS
1. Fact Sheet for Pet Owners and Veterinarians about Potential Adverse Events Associated with Isoxazoline Flea and Tick Products.
2. Bartonella is Everywhere, so Why Don't We Know More About It?
3. Collective Nouns for Birds,
Fast Facts
The FDA is alerting pet owners and veterinarians of the potential for neurologic adverse events in dogs and cats when treated with drugs that are in the isoxazoline class.
The FDA-approved drugs in this class are Bravecto (fluralaner) tablets for dogs, Bravecto (fluralaner) topical solution for cats and dogs, Nexgard (afoxalaner) tablets for dogs, Simparica (sarolaner) tablets for dogs, Credelio (lotilaner) tablets for dogs, and Revolution Plus (selamectin and sarolaner) topical solution for cats. These products are approved for the treatment and prevention of flea infestations, and the treatment and control of tick infestations. Revolution Plus is also approved for prevention of heartworm disease, treatment and control of ear mite infestations and some gastrointestinal parasite infections.
Although these products can and have been safely used in the majority of dogs and cats, pet owners should consult with their veterinarian to review their patients’ medical histories and determine whether a product in the isoxazoline class is appropriate for their pet.
What should I know?
The FDA considers products in the isoxazoline class to be safe and effective for dogs and cats but is providing this information so that pet owners and veterinarians can take it into consideration when choosing flea and tick products for their pets.
Isoxazoline products have been associated with neurologic adverse reactions, including muscle tremors, ataxia, and seizures in some dogs and cats; Although most dogs and cats haven’t had neurologic adverse reactions, seizures may occur in animals without a prior history; Many products are available for prevention and control of flea and tick infestations. You can discuss all options with your veterinarian to choose the right product for your pet.
What products are in the isoxazoline class?
The FDA-approved drugs in this class are
Bravecto (fluralaner) tablets for dogs
Bravecto (fluralaner) topical solution for cats and dogs
Credelio (lotilaner) tablets for dogs
Nexgard (afoxalaner) tablets for dogs
Simparica (sarolaner) tablets for dogs
Revolution Plus (selamectin and sarolaner topical solution) for cats
These products are approved for the treatment and prevention of flea infestations, and the treatment and control of tick infestations.
What should I do if my pet has an adverse drug event while using an isoxazoline product?
If your dog or cat experiences any adverse event while using an isoxazoline product, first consult your veterinarian.
The FDA continues to monitor adverse drug event reports for these products and encourages pet owners and veterinarians to report adverse drug events. You can do this by reporting to the drugs’ manufacturers, who are required to report this information to the FDA, or by submitting a report directly to the FDA.
To report suspected adverse drug events for these products and/or obtain a copy of the Safety Data Sheet (SDS) or for technical assistance, contact the appropriate manufacturers at the following phone numbers:
Merck Animal Health (Bravecto): 800-224-5318
Elanco Animal Health (Credelio): 888-545-5973
Boehringer Ingelheim (Nexgard): 888-637-4251
Zoetis (Simparica, Revolution Plus): 888-963-8471
If you prefer to report directly to the FDA, or want additional information about adverse drug experience reporting for animal drugs, see How to Report Animal Drug Side Effects and Product Problems.
Pet owners and veterinarians who have additional questions can contact AskCVM@fda.hhs.gov or call 240-402-7002.
Bartonella is Everywhere, So Why Don’t We Know More About It? - North Carolina Health News
Bartonella is a bacteria transmitted by fleas, ticks, animals, even spiders, but few people know about it. New methods for diagnosing it are showing it’s more common than previously thought.
By Stephanie Soucheray
An N.C. State professor says Bartonella infection is one of the most important untold medical stories.
Ed Breitschwerdt, a professor of veterinary sciences at North Carolina State University, keeps waiting for the tipping point. For the last 30 years, Breitschwerdt has been studying Bartonella, a genus of bacteria found in animals, ticks and humans.
“It’s frustrating,” said Breitschwerdt. “I believed we would hit a tipping point two years ago with this.”
Vectors of Bartonella infections include fleas, body lice, and sand flies.
Laura Hopper’s tipping point came in 2006, when she was 15 years old. The Raleigh teen lost her peripheral vision. She next began to suffer bouts of joint and muscle pain and numbness in her hands. Then came the headaches, memory loss and hallucinations.
“As a mother, it’s so hard to watch your child have all these symptoms,” said Maria Hopper. “It was a couple years of going to all kinds of doctors.”
But no neurologist, rheumatologist or psychiatrist could explain all of Laura’s symptoms. And it wasn’t until 2008, when the Hoppers read a news article about Bartonella and Breitschwerdt’s work, that a lightbulb went off in their heads.
Though people have known of cat scratch disease – the most public of the human diseases caused by Bartonella infection – for more than 100 years, Breitschwerdt said he’s convinced that Bartonella is the stealth cause of many neurological, inflammatory and chronic diseases in humans.
And, unlike Lyme disease, another tick-borne illness that can cause an array of distressing symptoms, Bartonella is right in the backyard of most North Carolinians.
“It’s a medically important bacteria in animals and humans in the state. If you took every stray cat along the coast of North Carolina, three quarters of them would have Bartonella,” said Breitschwerdt. “That’s because the bacteria is commonly transmitted to animals by fleas.”
He said that, historically, vets have considered common cat flea a nuisance but have under-appreciated it as a disease vector. For several years, Breitschwerdt has seen all sorts of animals and mites, ticks, fleas and even spiders test positive for Bartonella.
“Animals are the primary reservoir for the Bartonella species,” he said.
Breitschwerdt has worked with the One Health Commission, a collective that looks at the links between environmental, human and animal health. Though his professional and personal life has been guided by his care for animals, his most recent work is geared towards detecting and treating Bartonella infection in humans.
The recovery process:
The Hoppers contacted Breitschwerdt at a fortunate time: He was developing new human diagnostic method for Bartonella. Laura tested positive, and after three courses of months-long antibiotic treatments, her symptoms have all but disappeared.
“By the end of the first cycle [of antibiotics], the feeling in her hands came back,” said Maria. “By the end of the second cycle, hallucinations stopped.” Though Laura still suffers some muscle pain, she considers herself 80 to 90 percent healed.
If the bacteria is positively detected, treating Bartonella infection is a daunting task for even otherwise healthy patients
“You cannot float humans or horses in enough Doxycycline to kill this bacteria,” said Breitschwerdt. Treatment, such as Laura’s, requires weeks of multi-antibiotic therapies.
 Dr. Ed Breitschwerdt has found himself on the front lines
Dr. Ed Breitschwerdt has found himself on the front lines
of an epidemic no one has heard of. Image courtesy NCSU.
Laura was also lucky in that she tested positive for Bartonella immediately.
A patient infected can have a negative test on a Monday and positive test by Wednesday.
“People are tested several times, but Bartonella can hide in the body,” Breitschwerdt said.
That’s because an animal scratch or bug bite (or a vet’s needle stick) results in Bartonella infection in red blood cells and endothelial cells, which line blood vessels. The bacteria can “hide out” for many infectious cycles, causing symptoms and eventually affecting every organ system in the body.
Most people can clear Bartonella from their bloodstreams effectively. But among the subset of people who can’t eliminate the bacteria, help in mainstream medicine will be difficult to come by.
“I often talk with veterinarians who have these vague complaints – who say they’ve been sick for weeks or months,” said Breitschwerdt.
Many of the vets receive diagnoses of Lyme disease, chronic fatigue, rheumatoid arthritis, or are sent to a psychiatrist and told their symptoms are untreated depression. But Breitschwerdt cautions them to get tested for Bartonella.
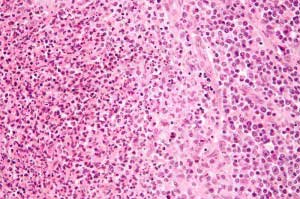 Highly magnified image of a lymph node infected with Bartonella henselae. Image courtesy Nephron, WIkemedia Creative Commons
Highly magnified image of a lymph node infected with Bartonella henselae. Image courtesy Nephron, WIkemedia Creative Commons
Breitschwerdt has ventured into industry with Galaxy Diagnostics, a company he founded to offer Bartonella testing kits to doctors. The company launched into human testing two years ago, and has received orders from 300 doctors across the country.
At this stage, said Amanda Elam, Galaxy’s president, the company’s goal is to educate people about Bartonella.
“We’re dong continuing medical education courses, working with people in public health and doing education with veterinarians,” she said. “I’d really like the medical community to keep an open mind about this.”
While Breitschwerdt waits for the public tipping point for Bartonella, he said he too is focused on disease education.
“It takes 10 years before something added to the medical textbooks gets widely spread in practice,” he said. “We’re working on changing those textbooks.”
Bartonella is Everywhere, So Why Don’t We Know More About It?
December 5, 2013 by Editor

