XXVI, Issue 1, February 2022
Page 12 previous page
next page
SOME HEALTH & SCIENCE NEWS
Fiddle Dee Dee
1. Xylitol is highly toxic to dogs - watch your toothpastes.
2. First treatment for the control of pain associated with osteoarthritis in cats and the first monoclonal antibody (mAb) new animal drug approved by the FDA for use in any animal species.
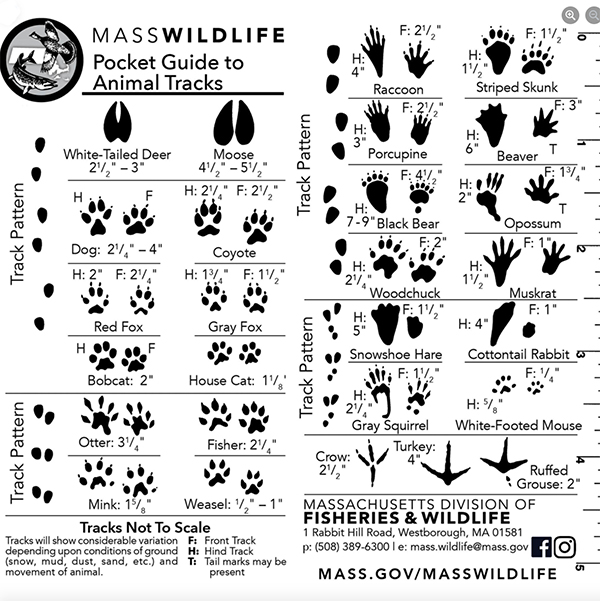
3. Animal Tracks in the snow.
Xylitol – Highly Toxic to Dogs
A friend recently had a terrible scare with a dog who ate a homemade cinnamon bun and got hideously ill; it turned out that the glaze on the bun was made with an artificial maple syrup that contained xylitol.
You may have heard that xylitol is toxic to dogs, and that you should never leave sugarless gum or mints that may have xylitol in them anywhere dogs can get them. (This includes in your purse or backpack, in the car, on your bedside table, or anywhere else your dog may have access to.) But are you aware how many MORE foods, medicines, supplements, and oral health products contain xylitol?
Xylitol, also known as “birch sugar” or ”wood sugar” (it’s made from birch and other wood products), is more and more commonly used in products for humans. It’s used in candies and baked goods meant for diabetics, as it sweetens foods in a way that does not cause an increase in a human’s blood glucose or insulin levels. But its use is not always called out as being appropriate for diabetics; increasingly, it’s used in regular baked goods, because it’s heat-stable (it doesn’t caramelize like regular sugar does).
It’s commonly found in:
- Toothpastes, mouthwashes, breath mints.
- Cough syrup and cough drops.
- Children’s and adult chewable vitamins.
- Supplements and over-the-counter medications. (One friend noticed it on the label of the melatonin supplement she takes to help her sleep; imagine if she left the bottle on her bedside table and one of her dogs helped themselves to the bottle?)
- “Skinny” or low-calorie ice cream.
- “Low-calorie” desserts of any kind (cookies, cakes, “energy” bars).
- Peanut butters and other nut butters. (This last one is particularly scary, as many people use peanut butter to “stuff” their dogs’ Kong or other food-puzzle toys. Always check the label of nut butters and any other food you use in a Kong, Toppl, or other food-dispensing toy!)
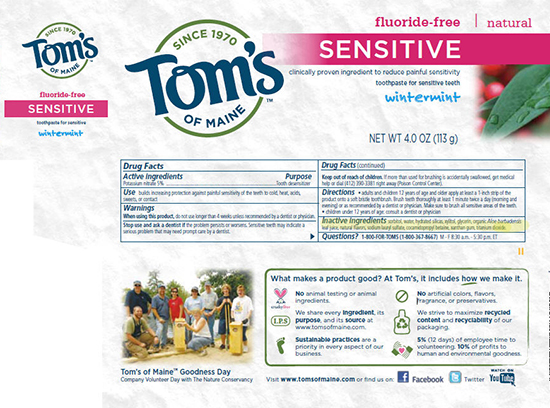
- Editor {I found that Arm & Hammer toothpaste is one that has no sweeteners}
It also doesn’t take very much xylitol at all to seriously sicken or kill a dog. According to the U.S. Food and Drug Administration, symptoms of xylitol toxicity in a dog include vomiting, followed immediately by symptoms associated with the sudden lowering of your dog’s blood sugar, such as decreased activity, weakness, staggering, incoordination, collapse, and seizures.
In dogs, xylitol is quickly absorbed into the bloodstream, and may result in a potent release of insulin from the pancreas. This rapid release of insulin may result in a rapid and profound decrease in the level of blood sugar (hypoglycemia), an effect that can occur within 10 to 60 minutes of eating the xylitol. Untreated, this hypoglycemia can quickly be life-threatening.
The FDA advises: “If you think your dog has eaten xylitol, take him to your vet or an emergency animal hospital immediately. Because hypoglycemia and other serious adverse effects may not occur in some cases for up to 12 to 24 hours, your dog may need to be hospitalized for medical monitoring.”
Prevention is key
The best way to prevent your dog from an accidental poisoning is to not buy products that contain xylitol, so they just are never in your car or house. But if you do have mints, toothpaste, cookies, or anything else in your home that contains xylitol, you must manage its presence in your possession like you would a loaded gun in a house full of toddlers. Keep any item –including toothpaste! – in a closed cabinet where the dog cannot possibly reach, never just on a kitchen or bathroom counter that a dog might be able to jump up and reach. If your dog is not a “counter surfer,” you may tend to be casual about items like toothpaste in the bathroom or mints on the coffee table. But a guest’s dog may be different – and all counter-surfers start somewhere, with some food item. You’d hate for your dog’s first foray into helping himself to some xylitol-containing food or supplement to be his very last meal ever.
Lastly, bipartisan legislation (called the Paws Off Act of 2021) that would require manufacturers of any product containing xylitol to include a warning label has been introduced in Congress. You can find more information and support the Paws Off Act by contacting your representative here.
FDA Approves Novel Treatment to Control Pain in Cats with Osteoarthritis, First Monoclonal Antibody Drug for Use in Any Animal Species
Today, the U.S. Food and Drug Administration approved Solensia (frunevetmab injection), the first treatment for the control of pain associated with osteoarthritis in cats and the first monoclonal antibody (mAb) new animal drug approved by the FDA for use in any animal species.
Frunevetmab, the active ingredient in Solensia, is a cat-specific monoclonal antibody (a type of protein) designed to recognize and attach to a protein called nerve growth factor (NGF) that is involved in the regulation of pain. When frunevetmab binds to NGF, it prevents the pain signal from reaching the brain.
“Treatment options for cats with osteoarthritis are very limited. Advancements in modern veterinary medicine have been instrumental in extending the lives of many animals, including cats. But with longer lives come chronic diseases, such as osteoarthritis,” said Steven M. Solomon, M.P.H., D.V.M., director of the FDA’s Center for Veterinary Medicine. “Today’s approval marks the first treatment option to help provide relief to cats that are suffering from this condition and may significantly improve their quality of life. We also hope that today’s approval of the first monoclonal antibody by the FDA for any animal species will expand research and development of other monoclonal antibody products to treat animal diseases.”
Osteoarthritis is a degenerative condition of the joints in which the normal cartilage cushion in the joints breaks down. Eventually, the bones in the joint rub against each other, causing pain, decreased joint movement, and sometimes the formation of bone spurs or other changes in and around the joint. Osteoarthritis continues to get worse over time; however, Solensia can help manage the pain associated with the condition to improve the cat’s quality of life.
Solensia is available only by prescription from a licensed veterinarian because professional expertise is required to properly diagnose pain associated with osteoarthritis in cats, administer the injection and monitor the safe use of the product, including treatment of any adverse reactions. Solensia is given through subcutaneous (under the skin) injection once a month and is dosed based on the weight of the animal.
Because of the difficulty in assessing chronic pain levels in cats, the FDA looked at whether the overall evidence supported the conclusion that Solensia was effective in controlling pain associated with osteoarthritis in cats. The effectiveness of Solensia was evaluated in two effectiveness studies using three clinical assessments that measured different aspects of pain associated with osteoarthritis in cats.
The two clinical trials were both masked, randomized, controlled field studies involving client-owned cats with clinical signs of osteoarthritis. The cats’ veterinarians assessed the cats based on orthopedic examinations before and after treatment. The owners of the cats provided baseline scores of their cats’ levels of impairment doing certain activities (such as jumping onto furniture, using the litter box or grooming), compared to the cats’ level of ability before they developed osteoarthritis. The owners then assessed their cats’ response after receiving treatment. Overall, the cats in the treatment group had better assessment scores than those in the control group.
The most common side effects seen in cats treated with Solensia included vomiting, diarrhea, injection site pain, scabbing on the head and neck, dermatitis and pruritus (itchy skin). These effects were relatively mild and did not require cessation of treatment.
Veterinarians should advise owners about the possible adverse events and side effects before using the drug. The FDA encourages cat owners to work with their veterinary team to report any adverse events or side effects potentially related to the use of any drug, including Solensia.
The FDA granted approval of Solensia to Zoetis Inc.
Page 12 previous page
next page